What is occlusion?
S Davies R M J Gray
In this part, we will discuss:
- What ‘occlusion’ is
- Why occlusion is important
- The significance of ‘ideal occlusion’
Abstract
The aim of this series of papers is to explore the role of occlusion in dental practice. The range of opinion in the dental profession as to the importance of occlusion is enormous. It is very important that the profession in general and practicing dentists in particular have a balanced view of occlusion. This is more important than every patient having a balanced occlusion. The fact that the study of occlusion is characterized by extremes makes it confusing and possibly difficult for individual dentists to find a philosophy which is in line with contemporary good practice supported by evidence from practice-based research.
Introduction
‘Occlusion’
There is no escape
Dentists cannot:
- Repair
- Move
- Remove
teeth without being involved in occlusion.

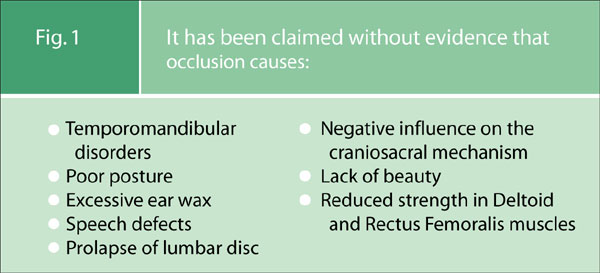
Conversely there is a body of opinion that considers occlusion to be such a central pillar in our working lives, and to be of such systemic import to the well being of our patients, that ‘occlusion’ takes on an almost mystic importance and attracts a cult like devotion (Fig. 1). This can lead some dentists to advocate occlusion as being the key to resolving or preventing a range of disorders far removed from the masticatory system, for example prolapsed lumbar discs. Often such enthusiastic favour is associated with a didactic prescription of ‘occlusal rules’ which must be adhered to in the treatment ofevery patient.
Figure 1: It has been claimed without evidence that occlusion causes:
The danger is that both of these approaches leads to inappropriate levels of patient care; patients suffer through either over or under treatment.
It is not surprising that these two extreme views co-exist so easily within a thinking profession because the one appears to provide the justification for the other. The ‘occlusion doesn’t matter’ group probably justify their reluctance to become ‘involved in occlusion’ on the grounds of what they perceive to be the exaggerated and unsubstantiated claims of the group who believe occlusion to be the central pillar of holistic care. This congregation of opinion in turn may be so frustrated by the apparent disregard of the study of occlusion that they are led to ‘gild the lily’ by overstating the importance of occlusion and then in the absence of what they perceive to be an inability ‘to see the obvious’ they go on to lay down rules.
It is the objective of this series of papers to explore the role of occlusion in dental practice in a manner based on reason. There is good and bad practice in occlusion as in other aspects of clinical dentistry: we wish, therefore, to establish the concept of Good Occlusal Practice, which is applicable to all disciplines in dentistry.
Guidelines of good occlusal practice
These should be guidelines not rules.
All patients are different, reacting to similar stimuli in different ways. So the detail of a patient’s individual needs can and should be left to the individual clinician. These Guidelines of Good Occlusal Practice should appear to be common sense and, upon reflextion, we hope that the reader will agree that they are obvious. We argue that any fog that has descended over this subject must be cleared, because no practising dentist can care well for their patients without having regard for good occlusal practice.
The importance of occlusion in dental practice
‘Occlusion’= Contacts between teeth
Occlusion can be defined very simply: it means the contacts between teeth.
Before describing the significance of the different ways in which occlusal contacts are made, occlusion needs to be put into context.
The masticatory (or stomatognathic) system (Fig. 2) is generally considered to be made up of three parts: the Teeth, the Periodontal Tissues, and the Articulatory System.
Figure 2: The masticatory system
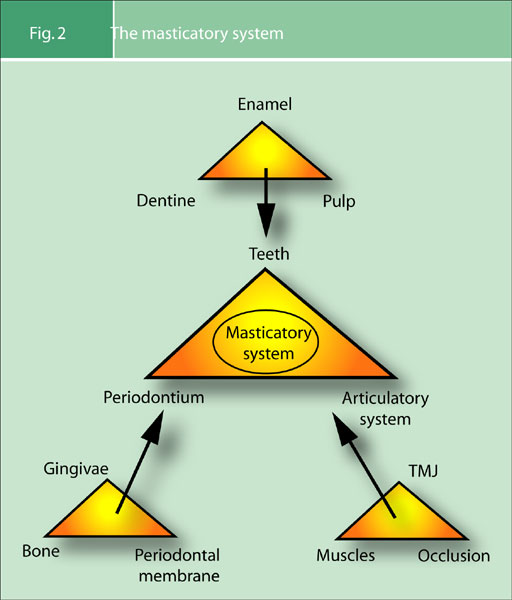
It is a common criticism of dentists that our dental schools ignore the third part of the masticatory system, the articulatory system, in their teaching. It appears that dentists feel that their time at university did not prepare them adequately in this area; and this view seems to be the case worldwide. The undergraduate dental education must, however, by necessity concentrate initially on the first two parts of this triumvirate, because the dental schools must produce newly qualified dentists who are able to treat patients. Only once the dental undergraduate has an understanding of the diseases that affect the dental and periodontal tissues (parts 1 and 2 of the masticatory system) can the schools start to allow the student to treat patients. So there is justification for the study of the articulatory system being considered to be the third area of study from a chronological point of view. But because of the inescapable fact that almost all dental treatment has an occlusal consequence, it is wrong to consider the study of the articulatory system to be less important than the first two parts of the masticatory system. Given the increasing quantity of knowledge to be amassed in the modern undergraduate course, it may be that those responsible for setting the dental undergraduate curriculum will not be able to cover the articulatory system as they would wish. Now that there is a universal acceptance of the need for continuing education, it may be more realistic to consider a comprehensive study of the articulatory system as the first mandatory element of a post graduate dental education. But the articulatory system is the biomechanical environment in which dentists provide treatment. Although it maybe, by necessity, the last to be learnt it is not less important than the other parts of the masticatory system.
Is the articulatory system a true system?
(Fig. 3a, b)
Figure 3: The articulatory system
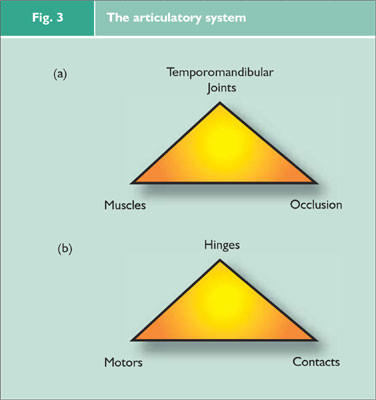 A system is defined as: ‘An assemblage that is connected or interdependent, so as to form a complex unity.'[OED] The articulatory system meets these criteria, so the answer to this question is: Yes.
A system is defined as: ‘An assemblage that is connected or interdependent, so as to form a complex unity.'[OED] The articulatory system meets these criteria, so the answer to this question is: Yes.
In this system one can imagine the temporomandibular joints as the hinges, the masticatory muscles as the motors and the dental occlusion as the contacts (Fig. 3b).
When viewed in mechanical terms (Fig. 3b) it is clear that the elements of the articulatory system are inescapably connected. Furthermore, it can be argued that they are obviously interdependent because a change in any part will clearly affect the other two parts (Fig. 4a), but this effect will not necessarily be adverse.
Figure 4: (a) Interconnections of the articulatory system (b) Interconnections of the masticatory system
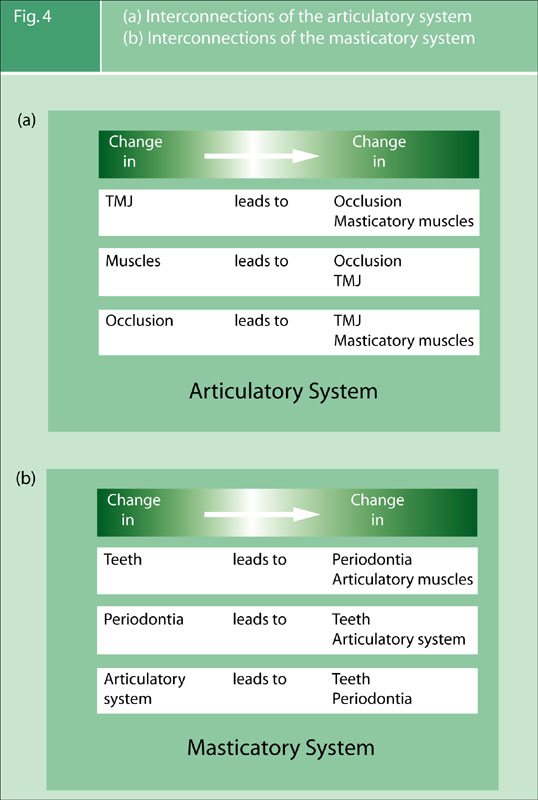
The same sort of analysis of the interconnection within the masticatory system can be made (Fig. 4 b).
The importance of ‘occlusion’ in dental practice is based primarily upon the relationships that it has within these interconnected biomechanical systems. When one considers how almost all forms of dental treatment have a potential for causing occlusal change, the need to establish what constitutes good occlusal practice is overwhelming and obvious.
Analysis of occlusion
Having stated that occlusion simply means the contact between teeth, the concept can be further refined by defining those contacts between the teeth when the mandible is closed and stationary as the static occlusion, and those contacts between teeth when the mandible is moving relative to the maxilla as the dynamic occlusion.
Static occlusion
The first essential question when considering a patient’s static occlusion is: ‘Does centric occlusion occur in centric relation?’
This question will be clarified after defining terminology, which has been a ‘red herring’ and has been the cause of enormous and sometimes acrimonious debate. We, also, have preferred terms, but do not feel that they are important.
Centric Occlusion (CO) can be described as the occlusion the patient makes when they fit their teeth together in maximum intercuspation. Common synonyms for this are Intercuspation Position (ICP), Bite of Convenience or Habitual Bite. It is the occlusion that the patient nearly always makes when asked to close their teeth together, it is the ‘bite’ that is most easily recorded. It is how unarticulated models fit together. Finally, it should be remembered that it is the occlusion to which the patient is accustomed ie the habitual bite.
The word
‘Centric’
is an adjective.
It should only be used to qualify a noun.
Centric what?
Centric Relation (CR) is not an occlusion at all. CR has nothing to do with teeth because it is the only ‘centric’ that is reproducible with or without teeth present. Centric Relation is a jaw relationship: it describes a conceptual relationship between the maxilla and mandible. All attempts to lay down rigid definitions of centric relation are plagued by the fundamental difficulty that there is no sure or easy way of proving that the locating criteria have been achieved.
Centric Relation has been described in three different ways: anatomically, conceptionally,2 and geometrically.
Anatomical
Centric Relation can be described as the position of the mandible to the maxilla, with the intra-articular disc in place, when the head of the condyle is against the most superior part of the distal facing incline of the glenoid fossa. This can be paraphrased as uppermost and foremost (Fig. 5).
Figure 5: Functional anatomy of the temporomandibular joint
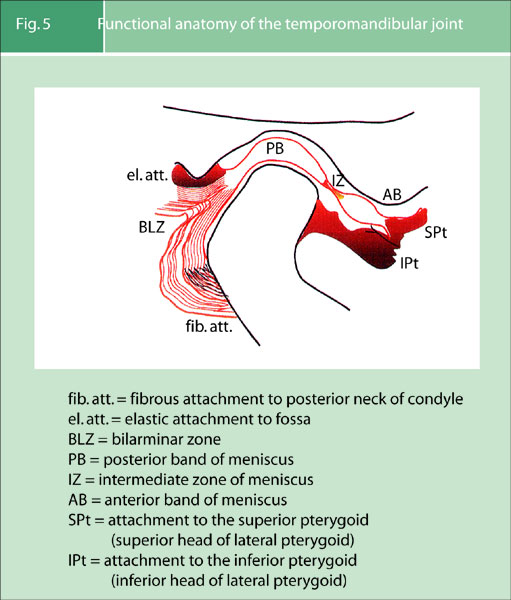
This is subject to debate. Some clinicians prefer the idea that centric relation occurs in an ‘uppermost and midmost’ position within the glenoid fossa; whereas very few people now support the idea that it is in an ‘uppermost and rearmost’ position. There is support for the uppermost and foremost hypothesis from a study of anatomy: the bone and fibrous articulatory surfaces are thickest in the anterior aspect of the head of the condyle and the most superior aspect of the articular eminence of the glenoid fossa. This is, however, of only academic interest and not of clinical significance as there is no reliable simple means of determining the exact position of the head of the condyle within the glenoid fossa.
Conceptual
Centric relation can be described as that position of the mandible relative to the maxilla, with the articular disc in place, when the muscles that support the mandible are at their most relaxed and least strained position. This description is pertinent to an understanding of ‘ideal occlusion’. This definition supports the concept of a ‘qualitative’ relationship between a jaw position and another element of the articulatory system.
Geometrical
Centric Relation can be described ‘as the position of the mandible relative to the maxilla, with the intra-articular disc in place, when the head of the condyle is in terminal hinge axis’.
In order to understand what this frequently used definition means it is easier, initially, to think about one side of the mandible only. The mandible opens by firstly a rotation of the condyle and then a translation which is downwards and forwards. Therefore, when the mandible closes the the terminal closure is purely rotational. At this phase of closure the mandible is describing a simple arc, because the centre of its rotation is stationary. This provides the ‘terminal hinge point’ (of rotation) of one side of the mandible; but because the mandible is one bone with two connected sides these two terminal hinge points are connected by an imaginary line: the terminal hinge axis. This axis is, therefore, envisaged by imagining the stationary, centers of rotation of each condyle whilst the mandible is moving only in the rotational phase of movement. It is the fact that the mandible is describing this simple arc, when the heads of condyle are in the terminal hinge axis which is of the most clinical significance. This will be discussed later, when the techniques for finding centric relation are presented.
Significance of Centric Relation
There may be arguments about the exact position of centric relation and on how that position is clinically best found. There is, however, a broad agreement between dentists who have studied this subject that there exists a reproducible position of the mandible relative to the maxilla, and that this position is reproducible irrespective of the guidance that the occlusal surfaces of the teeth may provide. Patients with no teeth still have a centric relation. Furthermore there is inter- and intra-operator reliability in finding it.
‘Freedom in centric’
‘Does Centric Occlusion Occur in Centric Relation?’
This is an essential question.
Another aspect of the static occlusion is the presence or absence of ‘freedom in centric’, this is also known as ‘long centric’.
As previously stated the word centric is an adjective and so strictly it should never be used without a defining noun. So this long established term would better read: Freedom in centric occlusion or long centric occlusion. Freedom in centric occlusion occurs when the mandible is able to move anteriorly for a short distance in the same horizontal and sagittal plane while maintaining tooth contact (Fig. 6b). Alternatively there will be no freedom in centric occlusion if either the front teeth or the posterior occlusion do not allow this horizontal movement (Fig. 6a).
Figure 6: (a) No freedom in centric occlusion (b) Freedom in centric occlusion
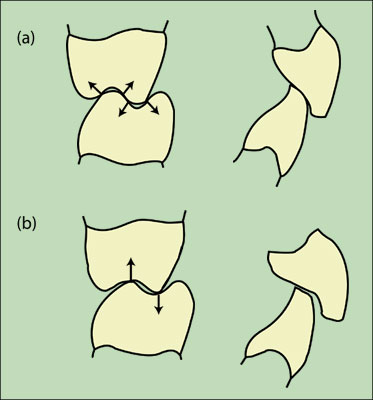
An easier way of imagining Freedom in Centric Occlusion is to state that if the front teeth hit together as hard or harder than the back teeth, then there is no freedom in that centric occlusion. Two common examples of occlusions that may not have this freedom are firstly those which have an Angles Cl II div (ii) incisor relationship and secondly when anterior crowns have been provided with palatal surfaces which are too thick.
In Figure 6a, there is no freedom in centric occlusion as the occlusal contacts ‘lock in’ the mandible to the maxilla. Whereas in Figure b the mandible can move anteriorly, for a short distance, in the same signal and horizontal plane.
Other aspects of the static occlusion that can be described are the extent of the posterior support, the Angle’s classification of the incisor relationship together with measurement of the overbite and overjet, and the existence of any cross bites.
The answer to the question: ‘Does Centric Occlusion occur in Centric Relation?’ is therefore essential, because it describes the relationship of the mandible to the maxilla when the teeth fit together.
Dynamic occlusion
Ideal Occlusion
Q. Who or what is it ideal for?
Posterior Interference
Q. Who or what is it interfering with?
The dynamic occlusion refers to the occlusal contacts that are made whilst the mandible is moving relative to the maxilla. The mandible is moved by the muscles of mastication and the pathways along which it moves are determined not only by these muscles but also by two guidance systems.
The posterior guidance system of the mandible is provided by the temporomandibular joints. As the head of the condyle moves downwards and forwards the mandible is moving along a guidance pathway which is determined by the intra-articular disc and the articulatory surfaces of the glenoid fossa, all of which is enclosed in the joint capsule.
If teeth are touching during a protrusive or lateral movement of the mandible then those (touching) teeth are also providing guidance to mandibular movement. This is the anterior guidance and this is provided by whichever teeth touch during excentric movements of the mandible.
No matter how far back these teeth are they are anterior to the temporomandibular joints and so a patient with a severe anterior open bite would still always have anterior guidance of their mandible, it could, for instance be on the second molars. Therefore, despite the ambiguity of the word ‘anterior’ in the term anterior guidance, it does not mean that the anterior guidance of the mandible is always on the front teeth. This definition differs from that given in some restorative textbooks, when the term anterior guidance is used to describe only those anterior guidences which involve front teeth.
Anterior guidance may be further classified. ‘Canine guidance’ refers to a dynamic occlusion that occurs on the canines during a lateral excursion of the mandible. A canine protected occlusion refers to the fact that the canine guidance is the only dynamic occlusal contact during this excursive movement.
Group function. In this type of anterior guidance the contacts are shared between several teeth on the working side during a lateral excursion. To qualify for the term ‘group function’, the contacts would be towards the front of the mouth and the most anterior of the group would be the earliest and hardest contacts. This would contrast with a ‘working side interference’, which infers a heavy or early occlusal contact towards the back of the mouth during an excursive movement. A ‘non working side interference’ is an anterior guidance on the back teeth on the non working side during lateral excursion. The working side is the side of the mandible towards which the mandible is moving during a lateral excursion. The non working side is the side of the mandible away from which the mandible is moving. These terms can be confusing when considering the temporomandibular joints, because it is the TMJ on the non working side which is moving the most.
One reason why restorative textbooks define anterior guidance as being solely the dynamic occlusal contacts between the front teeth is that it is generally considered to be more ideal if the anterior guidance is on those front teeth. Furthermore, the fact that the word ‘interference’ is used to describe an occlusal contact between back teeth infers that this anterior guidance is less ideal than others. This introduces the concept of ‘ideal occlusion’ and this raises two important considerations:
- If some occlusions are ideal, for what or for whom are they ideal?
- If occlusal contact between back teeth is deemed a posterior interference with what is it interfering?
Ideal occlusion
Let us examine this concept and question whether it has any useful function in routine clinical dentistry.
If two molars on the side from which the mandible is moving during an excursive movement can be deemed to provide a non working side interference, then what are they interfering with?
The posterior guidance of the mandible is provided by the temporomandibular joints. As the head of the condyle translates down the articular eminence of the joint on the non working side (which, paradoxically is the side that is moving the furthest) the mandible is being guided by this joint. If, as this is happening, a posterior maxillary and mandibular tooth hit against each other and because these two posterior teeth are close to the joint, then there is potential for the contact between these two teeth to influence or ‘interfere’ with the movement of the condyle within that joint. Contrast this with the situation, where the anterior guidance is provided not by posterior teeth which are close to the joint, but by front teeth which are further away; then the likelihood of ‘interference’ of condylar movement within the non-working side temporomandibular joint is less.
Anterior guidence, therefore, on back teeth, whilst still providing anterior guidence to the mandible, is described as a posterior interference because it may interfere with the posterior guidance system of the mandible, namely the temporomandibular joints. Posterior interferences are, therefore, considered to be a less ideal type of dynamic occlusion; and the term ideal relates to whether or not it is ideal for another part of the articulatory system: the temporomandibular joints (Fig. 7a). The anterior guidance provided by front teeth is potentially more ideal for the temporomandibular joints for the simple reason that it is further away from the temporomandibular joints. Consequently it can be argued that one aspect of the occlusion (anterior guidance) may or may not be ideal for another part of the articulatory system.
Figure 7: Occlusion is ideal for another part of the articulatory system
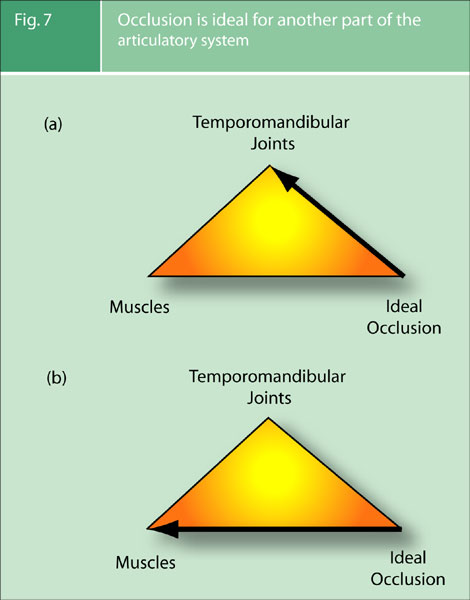
It is, also, potentially more ideal if the teeth fit together (centric occlusion), in a position of the mandible relative to the maxilla, with the disc in place, where the muscles supporting the mandible are at their most relaxed and least strained (conceptual description of centric relation). This establishes another criterion of the occlusion that can be considered ideal or not ideal for the other part of the articulatory system, namely the muscles of mastication (Fig. 7b).
Definition of ideal occlusion
There is no such thing as an intrinsically bad occlusal contact, only intolerable number of times for that patient at that time in their life to function or parafunction on it
This is given in established texts as:3
- The coincidence of Centric Occlusion in Centric Relation (CO = CR), when there is freedom for the mandible to move slightly forwards from that occlusion in the same sagittal and horizontal plane (Freedom in Centric Occlusion).
- When the mandible moves there is immediate and lasting posterior dissclusion (anterior guidence on front teeth)
It is presented in this section only after having considered for what or whom this type of occlusion is ideal, and the justification of why a particular type of occlusion could be considered as being potentially ideal for other parts of the articulatory system.
It is of paramount importance to appreciate that the term ‘ideal occlusion’ means something quite different from the term ‘correct occlusion’. To state that an occlusion is correct or wrong betrays a mechanistic approach to the subject. Patients are not machines and an occlusion can only be judged on the reaction that it produces in the tissues of the system in which it inter-reacts. That reaction will be infinitely variable between individuals and will in some contexts (ie TMD pain) vary within an individual with time.
Guidelines of Good Occlusal Practice should be established because they offer the most prudent way in which to provide dental treatment to one part of the system whilst avoiding a potentially adverse reaction in another.
The importance of ideal occlusion as a concept
1. Pretreatment examination and records
The first and most important reason for defining ideal occlusion is that it gives a benchmark against which patients’ occlusion can be measured. This needs to be done before, during and after dental treatment; especially in this increasingly litigious environment.
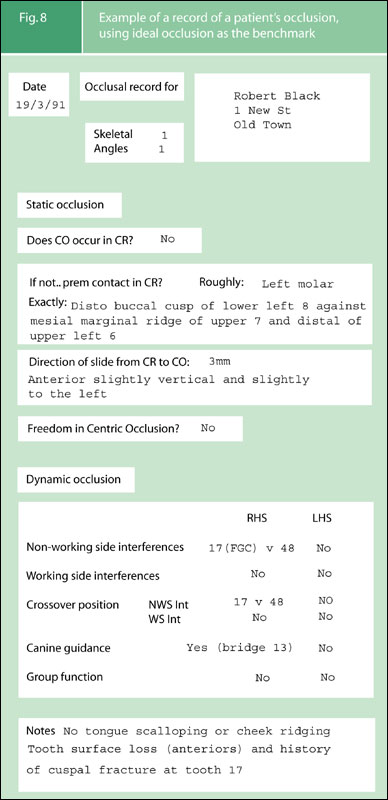
It is of paramount importance that dentists examine and record the pre-existing occlusion before providing treatment which involves changes to that occlusion. Study models would be a good way of doing this as long as they are mounted on an articulator in centric relation. At least the condylar guidance angles would also need to be correctly set so that the dynamic occlusion was recorded. This is not practicable for the vast majority of dentists. Alternatively and infinitely more easily notes can be made, which describe the patient’s occlusion. These notes use criteria of ideal occlusion as a benchmark. To record an occlusion using only the criteria of Angle’s classification is of very limited value, whereas to use the benchmark of ideal occlusion is considerable more informative Fig. 8.
Figure 8: Example of a record of a patient’s occlusion, using ideal occlusion as the benchmark
2. Treatment of Pain Dysfunction Syndrome (PDS)
Force > Resistance
- Reduces tissue resistance
- Causes failure
- Promotes pain/dysfunction
The second reason why ideal occlusion is an important concept is found in the long held view that the most important factor in the development of Pain Dysfunction Syndrome (PDS) is ‘the individual patient’s lack of adaptation to a less than ideal occlusion’. 4 This is not describing a causal relationship between a less than ideal occlusion and PDS, as different patients will have different thresholds of tolerances to occlusion, in fact the same patients have a different tolerance to their occlusions at different times. It is, however, the case that some patients, at some times, do react adversely to their less than ideal occlusions; and this can lead to pain and dysfunction.
For these patients the provision of an ideal occlusion is, therefore, one but by no means the only way of treating the condition. When an ideal occlusion is provided this should always be initially in a temporary and reversible way: that is a stabilization splint. The indications for the provision of an ideal occlusion in the patient’s natural dentition, for the treatment of PDS are very rare.
3. Conformative versus reorganized approach
In providing treatment with an occlusal element, one of the first questions to be decided in the treatment planning stage is whether the aim is to maintain the same occlusion during treatment. If the pretreatment occlusion is to be preserved, then the is described as ‘conformative approach’.5
Some dental treatment, such as most major restorative and all orthodontic treatment, will however, inevitably change the patient’s occlusion: this is known as the ‘reorganized approach’. It is, therefore, prudent to design an occlusion that is more ideal and so potentially better tolerated by the patient’s articulatory system.
Factors determining a patient’s reaction to an occlusion
As stated an occlusion can only be judged as being good or bad in relation to the reaction it produces in the patient’s tissues. In the same way that the danger of a substance can only be judged in relation to the concentration in which it occurs, a particular occlusal contact should be assessed in relation to the frequency at which it is made.
This is why bruxism is an important consideration in dentistry.
The ‘occlusion’ means the contacts between the teeth. The application of force from the muscles, through those occlusal contacts, results in load. Whether that load produces damage to tissues will depend on several factors:
- The resistance of the tissues and/or restoration.
- The magnitude of the force being applied.
- The frequency of the force being applied.
- The direction of the force being applied.
- The number of contacts transmitting that force.
Risk management
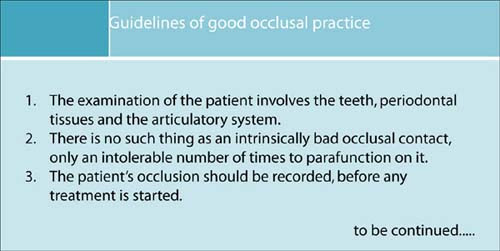
Guidelines of good occlusal practice
The purpose of guidelines of good occlusal practice is to reduce the risk of damage occurring to the interrelated tissues of the masticatory system, and so increase the chances of a healthy function. This will reduce the chances of disease, mechanical failure and dysfunction or pain. Dentists can positively influence these factors as part of their care.
The next section of this work will present the criteria for, and the technique of, a quick and simple occlusal examination. Thereafter, in subsequent sections, we will present the concepts of good occlusal practice in different disciplines of clinical practice. At the conclusion of each section further points will be added to create the cumulative Guidelines of Good Occlusal Practice.
References
- Smith B G N. Occlusion: 1. General Considerations. Dent Update 1991; 18: 141-145.
- Gray R M J, Davies S J, Quayle A A.Temporomandibular disorders: a clinical approach. pp20 BDJ publications, 1995 1997.
- Ash M M, Ramfjord S P.Occlusion 4th ed.: pp84-85. Philadelphia: Saunders,1995.
- Ramfjord S P, Ash M M.Occlusion 2nd ed.: p178. Philadelphia: Saunders, 1971.
- Wise M. Occlusion and restorative dentistry for the general dental practitioner. Br Dent J 1982; 152: 319-320.
- GDP, 73 Buxton Rd, High Lane, Stockport SK6 8DR; P/T Lecturer in Dental Practice, University Dental Hospital of Manchester, Higher Cambridge St., Manchester M15 6FH
- Honorary Fellow, University Dental Hospital of Manchester, Higher Cambridge St., Manchester M15 6FH
Correspondence to: S Davies1 73 Buxton Rd, High Lane, Stockport SK6 8DR
e-mail: stephen.j.davies@man.
David C. Suh DDS
Smiles are free and easy to give!
“We make a living with what we get, but we make a life with what we give!”
Sir Winston Churchill